Introduction
Poor Graft Function(PGF), defined as multilineage cytopenias in the setting of complete donor chimerism is a significant complication of allogeneic stem cell transplantation (alloSCT). Recently our group, in a published retrospective analysis of 929 patients, demonstrated that the following factors were associated with the development of PGF: Non matched sibling donor, ICU admission/ positive blood cultures within 1 st 30 days of alloSCT, severe graft versus host disease (GVHD), CMV viremia (Prabahran et al 2021). We extended our prior cohort study to validate risk factors previously associated with PGF and describe outcomes such as recovery from PGF, relapse and non-relapse mortality following a diagnosis of PGF.
Methods
This was a retrospective analysis of alloSCT recipients at our institution from 2017-2020. Patients 17 years and older were included. Patients who died prior to D60 of alloSCT were excluded as chimerism data was often not available prior to this timepoint. PGF was defined as follows: 1) ≥95% donor chimerism at last reading OR ≥95% CD3 negative chimerism; 2) ≥2 Lineage cytopenias defined as:
Thrombocytopenia :≤30x10 9 /L from D40-D60 OR ≤50 x10 9/L from D60 onwards; neutropenia requiring filgrastim support at any time post D40; Hb <80g/L. Factors associated with PGF were evaluated using a logistic regression, with development of PGF being the dependent variable. The predictive power of the subsequent logistic regression model was validated utilizing bootstrapping re-sampling procedure and testing of the concordance index (C-index). Variables associated with PGF were also evaluated in a cox-proportional model and coded as time-dependent covariates. Relapse and non-relapse mortality (NRM) were evaluated in a competing risk model from a landmark of 200 days post alloSCT, performed as per the method of Fine and Gray.
Results
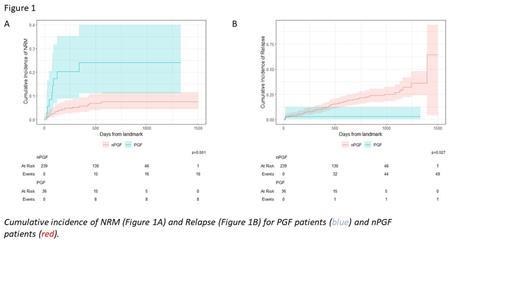
308 patients were included in the analysis of which 259 patients did not have PGF (nPGF) and 49 had PGF. Baseline variables of nPGF and PGF patients were matched for median age (53 versus 56 p=0.28), recipient sex (68% versus 65% male, p=0.74)), median CD34 dose (5.00 versus 5.2 x10 9/L p=0.49), donor source (p=0.12) and CMV serostatus (p=0.23). In multivariate analysis, ICU admission within 30 days (p=0.002), non-CMV viral infections (p=0.032) and GVHD (p<0.001) were associated with the development of PGF. The c-index of the model at baseline was 0.77 and 0.75 after bootstrapping validation indicating reasonable predictive performance of this model. ICU admission, non-CMV viral infections and GVHD were still significantly associated with the development of PGF when utilised as time dependent variables in a cox-regression model. Patients with PGF had worse 2-year survival compared to nPGF (60 versus 75% p=0.02). PGF patients without marrow recovery at last follow up had a 6-month OS of 20%. Twenty three out of 49 patients recovered marrow function at last follow up with a median duration of cytopenias of 142 days (51-789). The cumulative incidence (CI) of recovery was 44% and 53% at 1- and 2-years following onset of cytopenias respectively. From a landmark of 200 days (33 patients excluded due to death prior to this timepoint) PGF patients had a higher CI of NRM (Figure 1A =0.001) but lower CI of relapse (Figure 1B p=0.027) compared to nPGF patients.
Conclusions
PGF is strongly associated with early ICU admission, severe GVHD and non-CMV viral infections. Survival is inferior in patients with PGF particularly those with poor marrow recovery and this is mainly driven by non-relapse mortality. The lower CI of relapse in PGF is a novel finding of this study and may suggest a protective effect of PGF against the development of relapse but this finding requires further validation in external cohorts.
Disclosures
Chee:Otsuka: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Keros Therapeutics: Honoraria. Ritchie:Novartis: Honoraria, Research Funding; Amgen: Research Funding; Takeda: Consultancy, Honoraria; BMS: Research Funding; MSD: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal